Experience Hall
Effects of Process Changes on Emergency Department Crowding in a Changing World; An Interrupted Time-Series Analysis
Friday, September 22, 2023
1:30 PM - 2:00 PM PST
Has Audio

M.Christien van der Linden, PhD MsCE MsANP CEN RN (she/her/hers)
Research Coordinator Acute Care
Haaglanden Medical Center
The Hague, Zuid-Holland, Netherlands
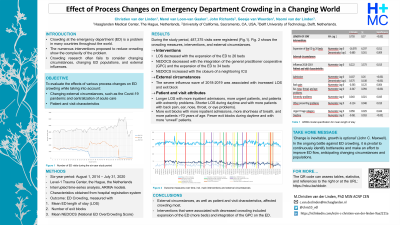
Purpose: : In this study, we assess the effects of process changes that we introduced during a six-year period. The process changes, such as the introduction of a general practitioner cooperative (GPC) at the emergency department (ED) and additional medical staff during peak hours, were expected to improve patient flow and decrease crowding. Meanwhile, centralization of emergency care took place, decreasing the number of EDs from three to one. We aim to provide insight into the effects of several process changes on crowding, patients’ ED length of stay (LOS), and number of exit blocks in the remaining ED, while accounting for changes in external circumstances and a changing population.
Design: : We assessed the effects of several process changes and external circumstances over a six-year period. Using a time series design, we described the effects on three crowding measures: ED patients’ LOS, a modified version of the National ED Overcrowding Scale (mNEDOCS) and the number of patients experiencing exit block. We extracted the following patient and visit characteristics from the hospital’s database for each registered patient: age, sex, presenting problem, triage level, day and time of the visit.
Setting:: The hospitals are located in the Netherlands. The facility delivers hospital care at three hospitals. Acute care was centralised from three EDs to two in 2017, and from two EDs into one in 2019. The remaining 34-bed ED serves as a regional level 1 trauma and acute neurovascular center and has a 29% admission rate.
Sample:: During the study period, 487,375 ED visits were registered: 50,201 in the ED that closed in month 33, 108,802 in the ED that closed in month 60), and 318,372 in the remaining ED.
Methods: : Crowding was defined as a mNEDOCS of >100. We calculated ED LOS and number of patients experiencing exit block (LOS >four hours for patients who need hospital admission. We summarized mNEDOCS scores, LOS and number of exit blocks per week and determined time points at which the various interventions and external circumstances took effect. We built an interrupted time-series model per outcome measure using ARIMA modelling to account for autocorrelation in the outcome measures. The statistical package for social sciences was used for the analyses. The regional medical research ethics committee exempted the study.
Results: : Longer patients’ ED LOS was associated with more inpatient admissions and more urgent patients. The mNEDOCS decreased with the integration of the GPC and the expansion of the ED to 34 beds, and increased with the closure of a neighbouring ED and ICU. More exit block occurred when more patients with shortness of breath and more patients > 70 years of age presented to the ED. During the severe influenza wave of 2018-2019, patients’ ED LOS and number of exit blocks increased.
Implications:: In the ongoing battle against ED crowding, it is pivotal to understand the effect of interventions, corrected for changing circumstances and patient and visit characteristics. In our ED, interventions which were associated with decreased crowding measures included expansion of the ED with more beds and integration of the GPC on the ED.