Experience Hall
Starting Early: Stopping Sepsis at the ED Door
Saturday, September 23, 2023
1:00 PM - 1:30 PM PST
Has Audio

Carrie Sinisko, BSN, RN, TNS, CEN
Emergency Department Outcomes Manager
Northwestern Medicine Delnor Hospital
Geneva, Illinois, United States
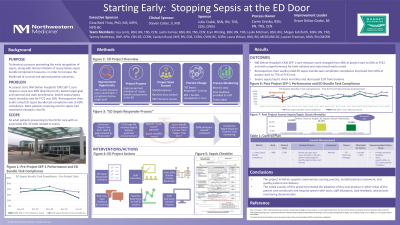
Objective: : With an understanding that the hospital's reported CMS SEP-1 quality measure score was below target goal and that a majority of patient cases with an associated ICD-10 code related to sepsis have treatment started in the ED, a nurse-led evidence-based practice (EBP) project was initiated with goals identified to improve the prompt recognition and rapid institution of resuscitative sepsis bundle component measures and to improve SEP-1 compliance.
EBP Model:: Recognizing the model's association with quality improvement and promotion of quality patient care delivery, the Iowa Model of EBP was utilized.
Setting:: The study setting is a suburban Level II trauma center located in the Midwest.
Participants:: The ED Outcomes Manager teamed with a facility Quality leader, ED Clinical Practice Specialist, Critical Care Clinical Practice Specialist, Rapid Response RNs, and Inpatient Outcomes Manager to define the quality improvement need and conduct the literature search. The ED Outcomes Manager teamed with the ED Clinical Practice Specialist to disseminate education and reminders to ED nursing and provider staff. ED Clinical Shift Coordinators reviewed key project updates and process expectations at shift huddles.
Methods: : Using the Iowa Model of EBP, the nurse-led project reviewed past ED SEP-1 data noting an average compliance rate of 60% to metric requirements. A literature review conducted confirmed the EBP guidance of completing sepsis bundle component tasks within 1 hour of sepsis time zero recognition aligns with optimal patient outcomes. The project multidisciplinary team created the ED Sepsis Responder process to improve SEP-1 compliance. The process included a checklist, page alert, ED internal announcement, admission handoff tool, and case feedback. Staff received process education and reminders. This new practice differs from general nursing practice with enhanced teamwork, tools, and communication to ensure SEP-1 criteria success.
Outcomes:: The EBP process changes initiated in the ED were a proven success. Baseline severe sepsis/septic shock mortality rate was 18% and improved to 14% (22.2% change). Sepsis bundle tasks initiated in the ED (lactate level, blood cultures, antibiotics started, fluid resuscitation) improved to a compliance rate of 77% from a baseline compliance rate of 60% (28.3% change). Overall compliance with the hospital's publicly reported SEP-1 quality measure score improved from 48% to 60% (25% improvement) with outperformance of national and state benchmarks noted. Staff feedback received regarding the process change reflected improvements in teamwork, communication, and awareness of critical clinical criteria.
Implications:: This project initiative supports autonomous nursing practice, multidisciplinary teamwork, and quality patient care delivery. Progression to sepsis may occur at any point during a patient's hospitalization. Early recognition and timely initiation of clinical interventions upon presentation to the ED for care allows for increased likelihood of survival and optimal patient outcomes. The recognized success of this project promoted the adoption of this process in other areas of the patient care continuum.