Experience Hall
Ambulance Offload Process Improves Offload Times
Saturday, September 23, 2023
11:30 AM - 12:00 PM PST
Has Audio

Tracy Page, DNP, RN, PHN
District Director of Emergency Services
Palomar Medical Center
Santee, California, United States
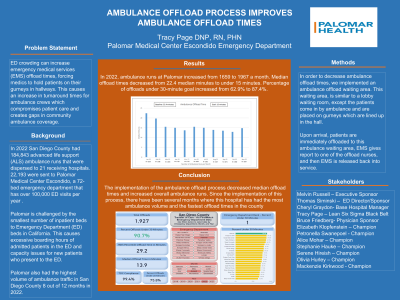
Aim: : Ambulance offload delay occurs when care of incoming ambulance patients cannot be transferred immediately from paramedics to staff in a hospital emergency department. This causes an increase in turnaround times for ambulance crews which compromises patient care and creates gaps in community ambulance coverage. Prolonged off-load times can also lead to delays in time to triage, time to physician, definitive patient care, and overall extended length of stay in the emergency department. The aim of this project was to decrease ambulance offload times.
Framework:: Lean Six Sigma
Setting:: A 72-bed emergency department/Level II Trauma Center that has over 100,000 ED visits per year in Escondido, CA.
Stakeholder Team:: Melvin Russell MSN, RN (CNO), Thomas Siminski MSN, RN (Director of ED), Cheryl Graydon BSN, RN (Prehospital Manager)
Methods: : In order to decrease ambulance offload times, we implemented an ambulance offload waiting area. This waiting area, is similar to a lobby waiting room, except the patients come in by ambulance and are placed on gurneys which are lined up in the hall. Upon arrival, patients are immediately offloaded to this ambulance waiting area, EMS gives report to one of the offload nurses, and then EMS is released back into service. Patients are triaged by the offload nurse and the offload physician evaluates the patient and places orders for treatment. The ambulance offload area is staffed by at least one nurse and an EMT. The nurse starts the ordered treatments for the patient and then moves on to the next patient who is waiting. This offload area is an alternative care space designated by our capacity and surge plan and is used when direct bedding is not an option. Like the lobby waiting area, these patients are not in a 4:1 nurse to patient ratio as the offload nurse is not assigned as this patient's primary nurse but is rather the nurse overseeing and facilitating getting treatments started until a room becomes available. The line continuously moves forward as rooms become available and the patient is then assigned a primary nurse who assumes care of the patient, documents the patient's assessment and continues the ordered treatments. Much like the lobby waiting room, rooms are assigned to patients based on acuity and based on the risk of life or limb-threatening emergency. To determine whether the ambulance offload waiting area would improve patient offload times, we compared offload time data from the six months immediately preceding our intervention to the 12 months immediately following implementation of the intervention.
Outcomes:: Ambulance runs increased from 1458 to 2131 a month over a year period. Median offload times decreased from 23.4 median minutes to 14.8 minutes. Percentage of offloads under 30-minute goal increased from 62.9% to 87.4%. Emergency department ranking amongst other facilities in the community increased from 10th to 1st.
Implications:: The implementation of the ambulance offload waiting area decreased median offload times and increased overall ambulance runs. It is suspected that more ambulances chose to come to our facility after this intervention due to less offload delay.