Experience Hall
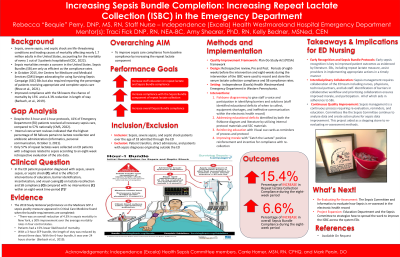
Increasing Sepsis Bundle Completion: Increasing Repeat Lactate Collection in the Emergency Department
Saturday, September 23, 2023
12:00 PM - 12:30 PM PST
Has Audio

Rebecca J. Perry, DNP, MS, RN (she/her/hers)
Assistant Teaching Professor / Emergency Nurse
Penn State University / Independence Health
Penn State University - Fayette Eberly Campus
Greensburg, Pennsylvania, United States
Aim: : Sepsis is a leading cause of mortality in the United States. Despite advances and evidence-based Sepsis Bundles, mortalities remain a concern. Sepsis Bundles are only as efficient as compliance rates. This project aims for patients to receive complete Sepsis care correctly EVERY TIME for EVERY patient.
Framework:: The project used Plan-Do-Study-Act (PDSA) framework.
Setting:: The project setting is a single Emergency Department in an acute care, non-profit, Magnet-recognized hospital system in Pennsylvania. The 578-bed system has three emergency departments that see numbers greater than 100,000 annually.
Stakeholder Team:: The project was approved by the Vice President of Patient Care Services. The project was developed with assistance from the Sepsis Committee and ED Medical Director. Gap analysis and data assistance was coordinated with nursing informatics, specifically a sepsis focused data analyst. Education was coordinated with the ED Educator. The ED manager assisted in delivery of the project. Emergency nurses and technical partners were educated and assisted in the implementation.
Methods: : This project's PICOT in the Emergency Department patient population diagnosed with sepsis, severe sepsis, or septic shock; what is the effect of interventions of education, barrier identification, incentivization, and visual cueing on lactate recollection and sepsis bundle compliance compared with no interventions within an eight-week time-period? This aim was to improve staff education on repeat lactate and sepsis bundles, increase compliance with repeat lactate collection, and increase overall sepsis bundle compliance. The design of this project was retrospective review and pre and post analysis. Eight weeks before the intervention and eight weeks during the intervention were used to record and store the lactate collection and sepsis bundle compliance rates. Data was collected with concurrent reviews, chart reviews, and collaboration with a sepsis data analyst. Data included sepsis, severe sepsis, and septic shock patients over the age of 18 admitted through the emergency department and excluded patient transfers, direct admissions, and patients with sepsis diagnoses originating outside the Department. The interventions were (1) Fishbone diagramming to give staff a voice and participation in identifying barriers and solutions, (2) addressing educational deficits identified by the fishbone and literature by utilizing protocol materials and SSC materials, (3) reinforcing education with visual cuecards as reminders of process and protocol, (4) and creating morale with “Catch the lactate” positive reinforcement and incentive for rewarding re-collection.
Outcomes:: Retrospectively repeat lactate collection rate for the site was 57% and overall sepsis bundle completion rate was 62%. Following implementation, repeat lactate collection rate climbed by 15.4% to 72.4%, and sepsis bundle compliance increased by 6.6% to 68.6% as well.
Implications:: Evidence demonstrates the significance of compliance, including repeat lactate measures, as influences on improved patient outcomes. Initiatives such as this contribute to a culture of learning as well as reinforcing the collaborative practice of evaluating and implementing change. The internal Sepsis Committee views the data results of increased compliance as an overall improvement in Sepsis Bundle compliance. The sepsis committee is assessing current reassessment protocols and exploring interventions to continue the increase in compliance and expand this initiative to other emergency departments within the system.