Experience Hall
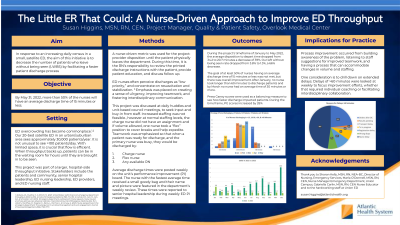
The Little ER That Could: Improving Throughput in a Satellite ER
Friday, September 22, 2023
1:00 PM - 1:30 PM PST
Has Audio
- SH
Susan Higgins, MSN, RN, CEN (she/her/hers)
Project Manager, Quality and Patient Safety
Overlook Medical Center
Highland Park, New Jersey, United States
Aim: : Our 20-bed satellite emergency department sees approximately 30,000 patients per year. It is not unusual to see over 100 patients a day. With limited space, it is crucial that flow is efficient. When throughput backs up, patients often wait hours to be brought in. Not only does this add to patients’ frustration, but can also result in adverse events and poor outcomes. We wanted to see if decreasing the time from patient disposition to ED departure, a nurse-driven metric, also decreased the number of patients who left without being seen (LWBS). The goal of the project was that in a six month period at least 50% of nursing staff would have an average discharge of 15 minutes or less.
Framework:: Using a PDSA model, we used a combination of education, motivation and coaching for process improvement. Tuckman’s Theory of Team Development was utilized to foster teamwork, cooperation, and trust among staff and providers.
Setting:: A 20-bed satellite ED in an urban/suburban area. It see approximately 30,000 patient visits/year.
Stakeholder Team:: The assistant nurse manager provided coaching, motivation and collected and posted data. The manager communicated our progress with senior hospital leadership weekly. The nurse educator conducted staff education including read and sign module and discussions at our unit based council.
Methods: : The time measured was from the provider's disposition to discharge the patient until the patient physically left the department, "disposition to discharge." A discharge report was run weekly and the data was used to find the average and median times for each nurse. Average discharge times were posted weekly and the nurse with the lowest average time won a small goodie bag and had their name and pictured featured in our "Week in Review". Monthly LWBS times were tracked and shared with staff and leadership. We also tracked our Press Ganey "Likelihood to Recommend" percentile as a balancing measure.
Outcomes:: The average disposition to discharge time fell from 34.2% to 20.7%, a decrease of 39.5%. We did not meet our goal of at least 50% of nurses discharging in less than 15 minutes, we saw an overall improvement. In January, 27.7% of nurses had discharge times between 16 and 30 minutes, 61% took between 30 to 60 minutes and 5.5% took longer than 60 minutes. After January, no nurse took longer than 60 minutes and by March no nurse had an average time longer than 30 minutes. Our Press Ganey percentile score went from 16% in January with a LWBS rate of 3.8% to a percentile score of 80% in May with a LWBS rate of 1.28%.
Implications:: Regardless of size or scope, any initiative will fare better when stakeholders agree on goals, aims, and expectations. Improving emergency department throughput is an evolving process, requiring collaboration and commitment. Fostering teamwork among staff with differing roles, priorities, and levels of experience is not easy, but can be accomplished when everyone focuses on the most important goal, providing a safer and more agreeable experience for the patient.